Please note we are in the process of updating this information to reflect the newly revised Mapping HIV Criminalization Laws in the U.S., CHLP (2025). Please refer to that document for the most up-to-date information.
While we have made every effort to ensure that this information is correct and current, the law is regularly changing, and we cannot guarantee the accuracy of the information provided. This information may not be applicable to your specific situation and is not, and should not be relied upon, as a substitute for legal advice.
HIV Criminalization Laws in the U.S.
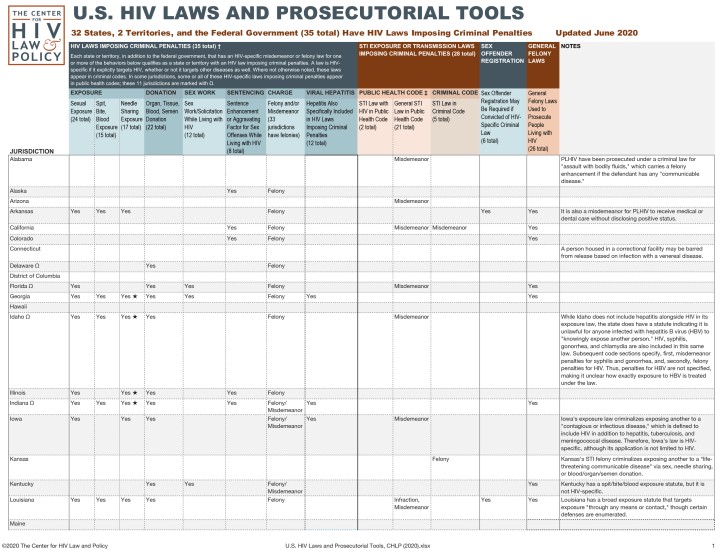
Pennsylvania has HIV-specific criminal statutes.
For detail on the selected state law and cases interpreting it, see Pennsylvania: Analysis & Codes, an excerpt from CHLP’s recently updated compendium of HIV- and STI-related criminal laws and civil laws relating to public health control measures in all 50 states, the military, and U.S. territories. To view the publication in its entirety, see HIV Criminalization in the United States: A Sourcebook on State and Federal HIV Criminal Law and Practice. Methodology is explained in the Introduction (page 5).
People living with HIV (PLHIV) or hepatitis B who are incarcerated face increased penalties for exposing others to their bodily fluids, including saliva.
It is a felony for PLHIV to engage in or solicit prostitution.
PLHIV have been convicted under Pennsylvania’s general criminal laws for various types of conduct, including failing to disclose their HIV status to sexual partners.
State Guidelines on Health Care Workers with HIV
We currently are in the process of reviewing and updating our resources and summaries related to health care workers and disclosure. In the meantime, please do not rely on this information as current, and get in touch with CHLP with any questions.
“Individual Health Care Provider” means a physician, nurse, emergency medical services worker, chiropractor, optometrist, psychologist, nurse midwife, physician assistant, dentist or other person, including a professional corporation or partnership, providing medical, nursing, drug or alcohol rehabilitation services, mental health services, other health care services or an employee or agent of such individual or an institutional health care provider.
Voluntary testing.
Infected HCW should notify prospective patients before patient undergoes exposure-prone procedure. Retrospective notification of patient is only indicated if evidence of significant exposure has occurred and should be conducted only after ERP has had an opportunity to assess risk.
Limiting the practice of infected HCW is not necessary or justified unless (i) there is evidence that such worker poses a threat to his/her health or safety or to the health or safety of others and (ii) that direct threat cannot be eliminated or reduced to a medically acceptable level with reasonable accommodation—such a direct threat should be based strictly on valid medical analysis and/or other objective evidence. Work restrictions are justified only if there is evidence that the infected HCW poses a significant risk of substantial harm to him/herself or others because of (i) his/her inability or refusal to meet basic infection control standards or because (ii) s/he is unable to care for his/her patients or otherwise perform essential functions of the job.
Minors' Access to STI and HIV Testing and Treatment
These summaries highlight key aspects of state laws governing the rights of minors to consent to testing and/or treatment for sexually transmitted infections (STIs) and HIV. Any such summary cannot capture the details and nuances of individuals state laws. Although roughly a third of the states permit health care providers to inform a minor's parents that their child is seeking STI-related services, none require it. Also, the law is fluid, and these summaries may not reflect recent legislative change in a particular state.
Every state in the country allows minors to consent to STI testing and care without parental approval, although a number of these set an age threshold for the right to consent without parental involvement. In these states, the minimum age ranges from 12 to 14 years of age.
As of the date of this posting, thirty-one states allow minors to also consent to HIV testing and treatment without parental approval.
HIV Testing
Unlike testing for most other infectious diseases, testing for HIV involves possible benefits as well as social, economic, and legal consequences that typically are not apparent or known to an individual considering testing. HIV-related testing is the gateway to health-preserving treatment; it also can be the basis of criminal prosecution for those who are sexually active, or relied on to exclude individuals who test positive for HIV from programs, employment, or insurance. Although state and federal laws prohibit much of this discrimination against people with HIV, the ability to enforce those rights usually depends on access to free legal services, which are increasingly limited and not available at all in roughly half of the states in the United States. Thus, the potential negative consequences of HIV testing at a particular time or location might inform an individual's decision of whether or when to get tested for HIV; or whether to test anonymously or through a "confidential" testing process that reports their test results and identifying information to the state but maintains the confidentiality of those results.
The American Medical Association has long defined informed consent as a process of communication between a patient and physician that results in the patient's authorization or agreement to undergo a specific medical intervention. Although informed consent is a legal concept rather than a medical one, many states use definitions of "informed consent" for purposes of HIV testing and medical procedures that in fact are inconsistent with the accepted legal definition, e.g., they do not require that an individual receive information or sometimes even notification that they are about to be tested for HIV. The Center for HIV Law and Policy (CHLP) accepts the legal and court-affirmed definition of informed consent; therefore, state protocols that call for "opt-out" testing (a patient is tested for HIV unless she/he objects) or that mirror general consent approaches are not counted as "informed consent" laws even in those instances where the state legislature has characterized their state law as requiring "informed consent." In short, CHLP does not consider or count laws that allow a patient's silence or general consent as granting authority to do confidential HIV testing as informed consent laws.
Pre-test information consists of an explanation of the test, including its purposes, potential uses, limitations and the meaning of its results.
Anonymous testing available at designated anonymous testing sites
Find the laws in a different state.
Copyright Information: CHLP encourages the broad use and sharing of resources. Please credit CHLP when using these materials or their content. and do not alter, adapt or present as your work without prior permission from CHLP.
Legal Disclaimer: CHLP makes an effort to ensure legal information is correct and current, but the law is regularly changing, and the accuracy of the information provided cannot be guaranteed. The legal information in a given resource may not be applicable to all situations and is not—and should not be relied upon—as a substitute for legal advice.