Published July, 2025
Achieving Greater Transparency Regarding Molecular HIV Surveillance: A Proposal to Move Beyond the Status Quo, Lumpkins et al, Open Forum Infectious Diseases (2025)
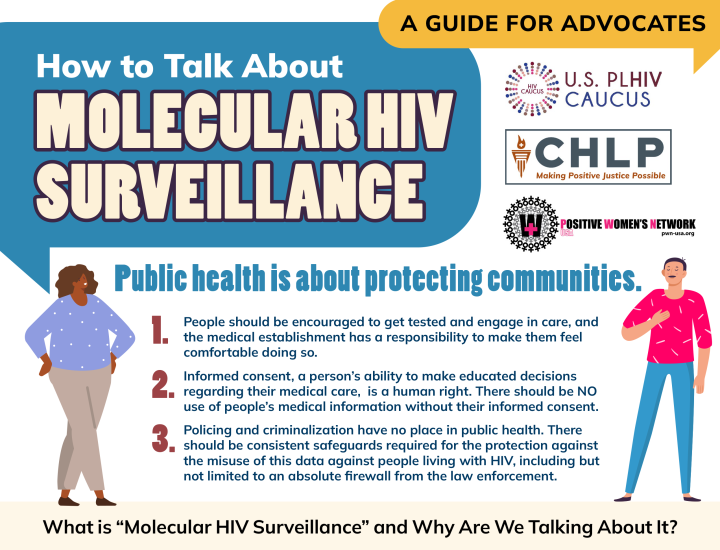
This journal article from Open Forum Infectious Diseases explores the ethical and practical challenges of using molecular HIV surveillance (MHS) to detect and respond to clusters of rapid HIV transmission. MHS relies on analyzing HIV genetic sequences, often collected through routine antiretroviral resistance testing, to monitor transmission networks and inform public health interventions. While this approach offers significant benefits for targeting prevention efforts, it raises concerns about data privacy, informed consent, and potential stigmatization of vulnerable communities. The authors emphasize the need for greater transparency and community engagement to maintain public trust and ensure ethical implementation of these surveillance systems.
A key component of the article’s analysis stems from SESAME (Study of Stakeholder Attitudes towards HIV Molecular Epidemiology), a project designed to examine ethical, legal, and social issues surrounding HIV molecular data use. Through SESAME, the authors convened a diverse working group—including scientists, public health officials, ethicists, and community advocates—to discuss how and when individuals should be informed about the use of their HIV sequence data. Insights from this group shaped the article’s central argument for a spectrum of disclosure approaches, ranging from minimal notification to full informed consent, as a way to balance public health goals with respect for individual autonomy and community trust.
Copyright Information: CHLP encourages the broad use and sharing of resources. Please credit CHLP when using these materials or their content. and do not alter, adapt or present as your work without prior permission from CHLP.
Legal Disclaimer: CHLP makes an effort to ensure legal information is correct and current, but the law is regularly changing, and the accuracy of the information provided cannot be guaranteed. The legal information in a given resource may not be applicable to all situations and is not—and should not be relied upon—as a substitute for legal advice.