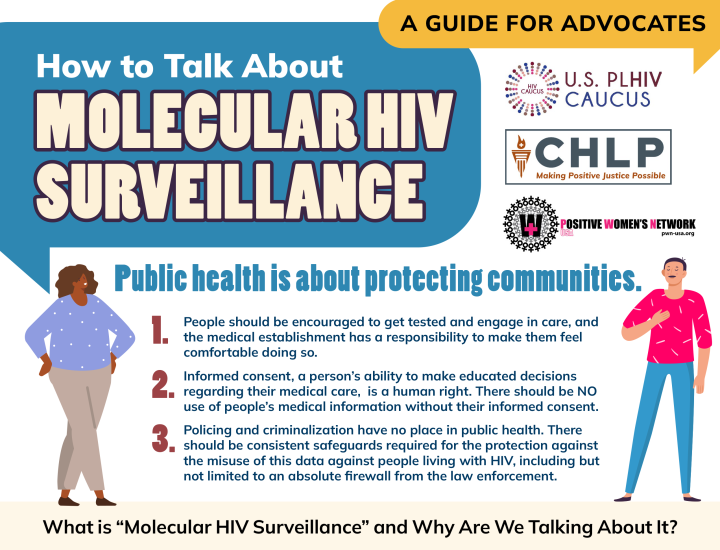
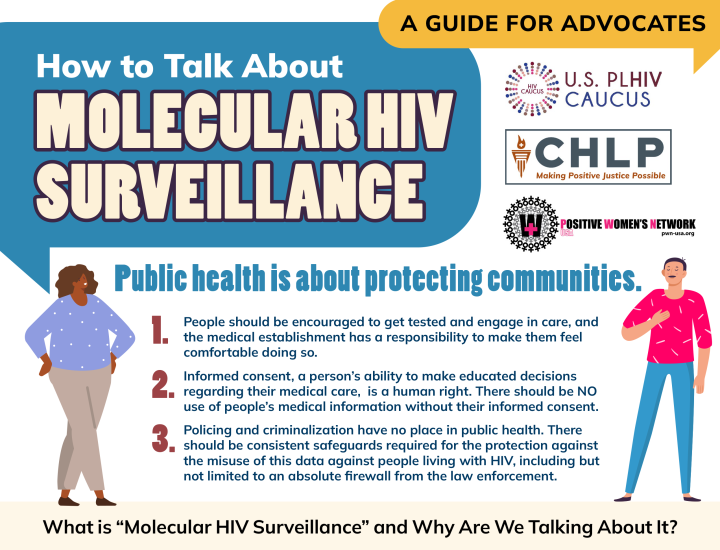
Testing and Informed Consent
In the United States, HIV testing is governed by a range of federal and state laws, common law principles, constitutional provisions, and various codes of ethics. State laws vary widely in the degree of protection provided. The concept of informed consent, achieved through the process of physician-patient communication, is a legal and ethical obligation spelled out by statute and case law in every state. Informed consent is a legal concept, not a medical concept, and it is central to values of individual autonomy and dignity. Informed consent is characterized by a process of communication between a patient and physician that results in the patient's authorization or agreement to undergo a specific medical intervention. Unlike testing for most other infectious diseases, testing for HIV involves possible risks, benefits, and consequences that may not be apparent to the patient.
This HIV Policy Resource Bank category includes materials focusing primarily on federal and state proposals related to the streamlining of the HIV testing process, from more patient-tailored pre-test and post-test counseling to the elimination of informed, documented consent. Also included are resources on the effectiveness of voluntary HIV counseling and testing approaches; the importance of voluntariness and autonomy in health care decision-making for marginalized populations, particularly people of color, immigrants, and non-native English speakers; and the role of HIV testing as a gateway to comprehensive HIV health care and support services.