Unsung Heroes: Dr. Jeffrey M. Birnbaum, HIV Physician, Brooklyn NY

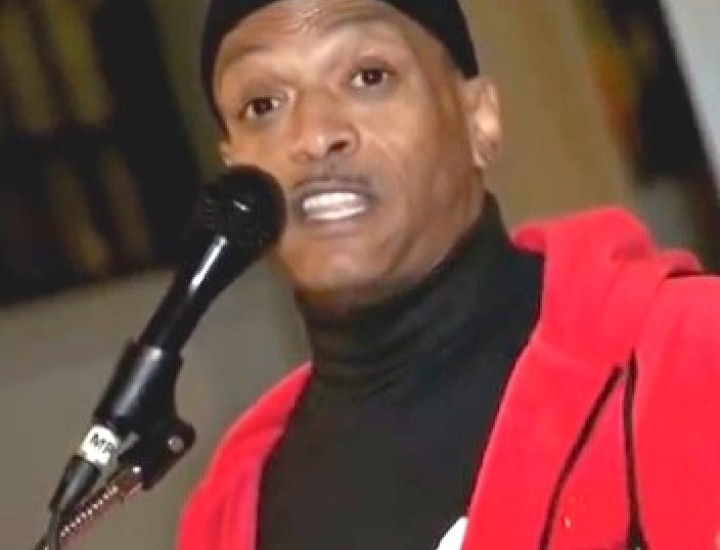
Dr. Jeffrey M. Birnbaum is an HIV physician at SUNY Downstate Medical Center who has worked exclusively with HIV-positive youth, ages 13- 24 years, since 1992. He is an Associate Professor of Pediatrics and Public Health and Executive Director of the Health & Education Alternatives for Teens (HEAT) Program at SUNY Downstate.
Dr. Birnbaum’s work with HEAT has been recognized by several prominent entities including the New York State Department of Health AIDS Institute which recognized his contributions with the 2012 Linda Laubenstein Award for excellence in HIV Care.
He is the author of several sets of clinical guidelines for clinicians who treat HIV-positive teens and he regularly mentors medical and public health students serving the HIV community across Brooklyn. Dr. Birnbaum has represented Downstate with his HIV expertise internationally, providing training sessions and consultation in Nigeria, Malawi, the Czech Republic, Poland, and Russia. He was interviewed by CHLP’s Andrea Sears.
Andrea Sears How did you become involved in HIV medicine and why did you choose that field?
Jeffrey Birnbaum I guess it was a moment in history. I had just finished my training. I had a Masters Degree in Public Health and was looking for something interesting to do. While I was actually looking for work overseas, the opportunity to work at the HEAT (Health and Education Alternatives for Teens) program, where I’ve been working since 1992, crossed my path. It just seemed like the challenge to rise to and I’ve been here since.
I’m trained as a pediatrician. While I was in my pediatric training and before that, all through medical school, it was the onset of the HIV epidemic. So I was in the right place at the right time and it just seemed like the thing I was going to do.
AS From that perspective what are the changes in HIV diagnosis, treatment and the life expectancy that you’ve witnessed over the course of your career so far?
JB It’s gone from literally being a death sentence to what we somewhat euphemistically refer to as a “life sentence”. Instead of dealing with impending death and despair over an untreatable illness, people with HIV now have a long-term, chronic, manageable disease, albeit one with a stigma. That’s the only thing that sets it apart from, say, diabetes and hypertension is that those diseases don’t have quite the emotional impact or stigma that HIV does.
AS You were involved in the Nushawn Williams case. How did you get involved in that case and what was your role there?
JB The Center for HIV Law and Policy asked me if I would be willing to provide expert testimony on his case. My opinion is that he’s already served his time for his original crimes. They aren’t holding him because of his crime. They’re holding him because he’s HIV positive and he makes for an easy slam-dunk case for prosecutors. They don’t want to be perceived as freeing someone who was painted as “public enemy number one” during an era when HIV treatment was not what it is today. They don’t want to be perceived as letting this “public menace” out. So they were going to do whatever they could to keep him confined when he’s already served his sentence.
What’s the crime? The crime that they’re holding him for, at this point, is being HIV positive. That’s not a crime in New York State. He was sentenced for statutory rape, whatever the exact charges were at the time, and he was convicted and he served his time for that already. Why are they keeping him in jail? Just for the fact that he’s HIV positive? That just didn’t sit right with me.
So I was invited to provide testimony, not so much about him, but about the infectiousness of HIV in the current world. I was there to provide testimony on whether somebody on HIV treatment is still infectious or not. Can they spread the disease? How can they still spread it? What if they’re on treatment, are they still infectious? So I gave testimony along those lines and really stuck to the information about that without necessarily delving into the particulars of his case although I had a brief conversation with him in the court conference room beforehand. He told me he was on treatment and that he currently had an undetectable viral load and past that I didn’t have much clinical information on him. So when I was questioned about it in court I spoke to the only information I had which is what he had told me in the conference room. But other than that I didn’t delve into other areas. I focused on the transmissibility of HIV and under what circumstances it would not be transmitted.
AS In 1998, when his trial was in full bloom, it got national attention. How did the Nushawn Williams case affect the relationship between doctors and their patients during the original trial and later when he was put in civil confinement?
JB Well, in terms of what we’re required to do today, we’re mandated to ask questions about sexual partners and if we get information about partners we’re required to report that. So part of the routine on an initial visit or going forward for that matter is we’re always trying to get partners to come in for testing. But if a partner comes in to get tested in the clinic we are required to share that information with the Department of Health on who the partner was and that we did in fact test the partner and give the results on the partner.
When we don’t do that, typically, the Department of Health will contact the HIV positive person themselves and say, “we’re the Department of Health, we’ve gotten your tests from the hospital and we’re trying to follow up with you about partners.” In terms of how that impacts our care, if the HIV positive person does not know that they’re going to be contacted by the Department of Health sometimes they can flip out over that and it can be quite distressing to them if they are not expecting such a call.
What I do with my patients is I try to collect the information for the Department of Health so that they don’t get these distressing, unexpected phone calls. I already have some rapport with the patient so I collect it for them and then I pass information on to the Department of Health. Much of the time, either at the initial visit or going forward after that, people are happy to give that information. It’s just when they’re caught off guard and not expecting a call that it can be traumatic to them. That’s a very sensitive issue for them.
AS Are patients warned or advised prior to testing that their results will not be confidential if they test positive?
JB It’s considered routine that before somebody gives consent they’re told that it’s one of the exceptions to confidentiality. The way I phrase it, “in the unlikely event that you test positive we’re obligated by law to share information with the New York City Department of Health and with the New York State Department of Health for the purposes of tracking the HIV epidemic.” That’s how I do it. And I’m sure the Department of Health does it that way as well. But in a lot of places when people get tested for HIV they’re not given much information. They’re handed a consent form or these days they’re giving verbal consent and people may not be fully informed, or it’s buried in a poster on the wall in the waiting room and is not explicitly stated. So I don’t know how well it’s being implemented but people are supposed to be warned beforehand.
AS Have you encountered patients who were afraid HIV could be used against them in court? That they may be accused of transmitting HIV to someone else?
JB It comes up all the time. And to be honest I’m not aware of any law in New York State where it’s criminal, but it comes up where people ask things like, “isn’t it illegal to have sex once you’re HIV-positive?” And they’ll have perceptions that anybody they have sex with is automatically going to be infected. Those are things that come up. People are rightly concerned about both infecting someone as well as maintaining their privacy around their own status. So those are things that become part of the routine conversation that you have with a patient’s when they’re first entering care.
It definitely opens a door for discussion about prevention of HIV transmission. Quite often when we tell them that by being on treatment they are in fact not infectious to spread HIV to other persons if their viral load is undetectable, for some people that’s an incentive to start HIV treatment. They sincerely don’t want to infect their partners and they didn’t know that there is a way that they could protect them. So it’s an incentive whether they disclose their status to their partner or not they can say to themselves in good conscience, “well I didn’t tell them but at least I protected them.”
AS What are the best things that doctors can do to assure their patients that they can actually protect themselves from state intrusion down the line?
JB I would say, in terms of good practice, having disclosure discussions frequently and early with their patients about whom they’re involved with and what the disclosure circumstances around an individual partner may be, and making that a part of routine care so that the information is out there would be a good thing. And that for the purposes of protecting themselves against state intrusion, if someone is engaging in a conversation with their doctor about how to protect their partners it shows due diligence on that person’s part, that they’re expressing appropriate concerns and it’s not, in legal terms, depraved indifference and that sort of thing.
Considering the fact that it is now New York State Department of Health policy that physicians should seek to get all their HIV patients to have undetectable viral loads to prevent the further transmission of HIV, getting any person with HIV to have an undetectable viral load is probably something that should protect patients from this type of state instruction. That assumes the state follows its own logic in this policy by not criminalizing someone’s HIV status.
AS What do you think the impact of the Nushawn Williams case has been on HIV criminalization? Has law enforcement or government been too quick to associate HIV status with criminal behavior? Has this made a link that just isn’t tenable?
JB Absolutely. It’s now a crime to have a disease. I mean there are lots of people who are HIV positive who never get tested. They may have suspicions, but they never get tested and they go around and have lots of unprotected sex, infect somebody and that’s not a crime, but the person who does know their status, and may be on treatment, and may be uninfectious – it’s considered criminal activity? That’s just crazy. That’s a way to perpetuate an epidemic in this country. Criminalizing HIV drives people away from HIV testing and care.
CHLP’s Unsung Heroes is a series of portraits included in The Fine Print blog of individuals who are contributing mightily, without fanfare, to keep our issues, needed agencies, and members of our communities alive.