The Body: Conflating Sexual Assault and HIV Criminalization

On April 4, CHLP attended a hearing of the Louisiana House Committee on the Administration of Criminal Justice in Baton Rouge. The hearing concerned modernizing the state’s criminal HIV exposure statute and fellow advocates from the Louisiana Coalition on Criminalization and Health (LCCH), including Robert Suttle, attended the hearing to give testimony. Robert spoke expertly about the personal toll of being criminalized and was joined by two medical professionals who testified in favor of modernizing the law.
Following them, representatives of the East Baton Rouge DA’s office presented highly stigmatizing testimony against modernizing the law that equated living with HIV and sexual violence and an intent to harm. This comingling of HIV status and criminality is a pervasive theme in our work to counter HIV criminalization laws. In this case, the DA’s office was happy to put forth stigmatizing theories and unfounded claims in order to preserve their ability to prosecute and punish.
In this article, Robert unpacks why sexual assault and sex-related crimes have no place in the discussion around HIV criminalization. His essay and our experience at the hearing make it clear what HIV advocates in Louisiana and around the country are up against, and why it’s so important that we persist in chipping away at these damaging arguments and antiquated laws.
Conflating Sexual Assault and HIV Criminalization
Apr 30, 2024
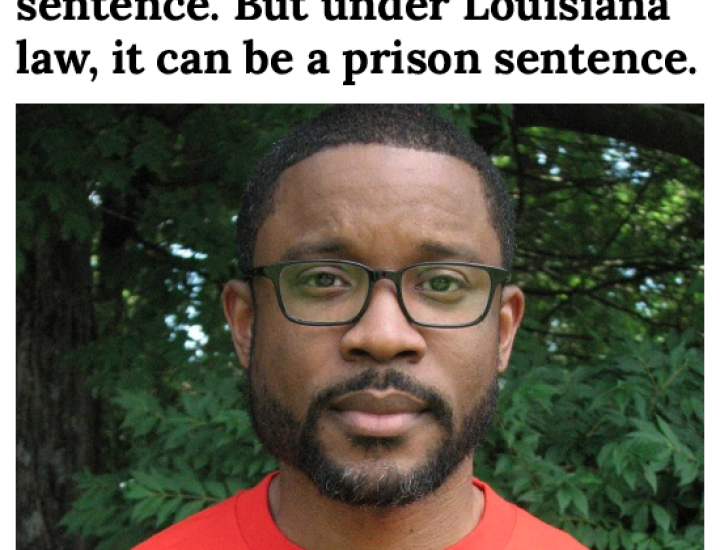
By Robert Suttle
On April 4, the Louisiana House Committee on the Administration of Criminal Justice held a hearing about modernizing the state’s criminal HIV exposure statute. As it currently stands, people living with HIV in Louisiana can be prosecuted for not disclosing their status before engaging in sex. This can happen even if they use condoms, are in treatment with antiretroviral therapy (ART) and are undetectable (#U=U) and incapable of passing the virus through sex, and if the seronegative partner is using pre-exposure prophylaxis (PrEP), which protects people who use it from acquiring the virus.
I attended that session to testify on the need to reform Louisiana’s existing HIV-specific criminal law in line with our modern-day understanding of science. However, during that same session, Kathleen Barrios―a representative of the East Baton Rouge district attorney’s office―presented oppositional testimony that conflated HIV with sexual violence.
Misinformation and Conflating HIV With Sexual Assault on the Legislative Record
During her testimony, Barrios mentioned a case from 2016 that involved a man living with HIV who raped a retired school teacher. She also presented misinformation about treatment with post-exposure prophylaxis (PEP).
“When we expose victims to this chronic disease,” she continued, “it is not un-traumatic for them even if they don’t end up with the disease. They still have to undergo prophylactic treatment [PEP]. And that is not a one-time treatment. They must follow up on that. They have to then continually be tested for the disease to make sure that they have not contracted a chronic disease.”
People who have been exposed to HIV who take PEP within 72 hours can stop HIV from taking root in their bodies. Like many treatments for sexually transmitted infections, PEP requires a once-daily oral pill for an extended period of time―in this instance, for 28 days. However, Barrios’ claim that people on PEP “have to then continually be tested for the disease” is false. People who initiate PEP are tested for HIV after they complete treatment and then again three months later.
This misinformation notwithstanding, Barrios went on to state, “That is a separate crime from the actual sexual assault, or the battery itself―that the victim is traumatized by. This statute, if you pass [this bill], it effectively repeals any kind of criminal penalty associated with doing something like that, because we’re reducing the penalty by 90%. We’re going from 10 years to one year.”
Following her testimony, Louisiana state Rep. Alonzo Knox asked, “In the scenario that you mentioned, where the rape took place: Would the rapist be charged for multiple crimes? Would he be charged for rape, and then, would he be charged for HIV and not on meds or HIV and on meds?”
Barrios explained that in the situation she mentioned, the assailant was convicted of three crimes: home invasion, second-degree rape, and intentional exposure to HIV. She noted that the woman he raped was treated with PEP and did not acquire HIV. She failed to mention that the assailant was a “60-year-old fifth felony offender”―as the court document described him―with a criminal history spanning more than 45 years.
Nor did she reveal that the assailant was sentenced to 25 years at hard labor for home invasion, 40 years at hard labor without benefit of probation, parole, or suspension of sentence for each of two counts of second degree rape, and 10 years at hard labor for “intentional exposure to AIDS virus,” with three of the sentences running concurrently. Contrary to Barrios’ claim that without the HIV exposure statute, “we’re reducing the penalty by 90%. We’re going from 10 years to one year,” given this assailant’s advanced age, he is all but guaranteed to die while serving hard labor in prison, whether the HIV criminalization charge is included or not.
As a follow-up, Knox asked, “Is it also your position that failure to disclose one is HIV positive to a sexual partner—is that a crime?” Barrios responded, “It’s not that it’s a failure to disclose, but if you fail to disclose and then you expose someone to HIV, yes, you could face criminal penalties for that.”
Knox closed his remarks by stating, “Whether they are on meds or not, for my own benefit and edification, I would want to make a decision if I would want to engage in sexual activity with someone with HIV.”
During his questioning, it seemed at first that Knox was in favor of looking at treatment as a means for disqualifying the HIV-exposure statute, until he affirmed that he would also want to know a potential sex partner’s serostatus regardless of their treatment status.
Editor’s note: Readers can watch the full exchange on video in Louisiana’s House of Representatives archive. Cue up to the 2:57:30 time stamp.
Barrios and Knox’s remarks were dispiriting because they perpetuate stigma and have been preserved in the official record without receiving a science-based challenge. Similarly, they conflate HIV nondisclosure with malicious intent―a frequent talking point from opponents of HIV criminalization reform―when nothing could be further from the truth. As I have written previously, if we want people to disclose their HIV status, we have to first make it safe for them to do so. And as the Centers for Disease Control and Prevention (CDC) notes in its brief about HIV criminalization, “These laws have not increased disclosure and may discourage HIV testing, increase stigma against people with HIV, and exacerbate disparities.”
The CDC goes on to recommend, “When a law meant to protect the public is not working as intended, is unjust, and may be hurting efforts to keep communities healthy, common solutions must be found to better meet public health and public safety goals.”
In light of April’s designation as Sexual Assault Awareness and Prevention Month, I think it is time to address sexual assault and sex-related offenses and why neither have any place in the discussion around HIV criminalization.
The Intersection of Sexual Assault and HIV Criminalization
“Sexual assault” and “sex-related offenses” are two distinct terms that refer to different aspects of illegal sexual behavior. Sexual assault generally refers to any non-consensual sexual act involving physical, verbal, or psychological coercion, manipulation, or force. On the other hand, “sex-related offenses” is a broader legal term encompassing all sexual crimes, including sexual assault, as well as certain consensual sexual activities deemed illegal under specific state laws. For example, HIV-specific criminal laws can and do prosecute people living with HIV for engaging in behaviors even when transmission is impossible: spitting on another person, giving oral sex. Understanding these definitions helps clarify the scope of legal and social discussions surrounding sexual violence.
When sexual assault and HIV criminalization intersect, they do so through multifaceted legal and social frameworks that significantly impact individuals’ rights, while perpetuating stigma and access to justice. Both areas involve deeply ingrained societal misconceptions and a legal apparatus that often does not serve justice or protect the rights of the vulnerable.
Marginalized communities, including LGBTQ+ individuals, women, Black, Indigenous, and other people of color, and those with limited access to health care and legal resources may experience intersecting challenges related to both sexual assault and HIV criminalization. These can include barriers to reporting assault, accessing health care and support services, and navigating the legal system.
Similarly, several commonalities exist between sexual assault and HIV criminalization, like:
- Stigmatization: Both survivors of sexual assault and individuals living with HIV face increased types of stigma-related experiences. This stigma can lead to social isolation and discrimination and can significantly impact the mental health and well-being of affected individuals.
- Legal and social challenges: Both groups often face an unjust legal system that inadequately protects their rights. For instance, survivors of sexual assault may struggle with proving non-consent, while those living with HIV might be prosecuted under laws that disregard the actual transmission risk or the scientific facts about HIV.
- Misconceptions and fear: Both areas are riddled with public fear and misconceptions that can lead to reactionary legislative practices and social ostracism and discrimination.
Stigmas and Disparities
Looking at the intersection of HIV and sexual assault from a legal perspective, we see that their association began to take shape in the late 1980s and early ’90s as the HIV/AIDS crisis unfolded. Laws were enacted that specifically addressed alleged HIV nondisclosure, perceived exposure, or transmission, often categorizing these actions within the framework of sexual assault despite significant differences in context and intent. This legal conflation has led to the enforcement of HIV criminalization in the U.S. in ways that many advocates and experts argue are scientifically unfounded and unjust, effectively punishing individuals living with HIV solely for their health status rather than any real intent to harm.
Today, misconceptions about HIV contribute to its characterization as a form of sexual violence, particularly concerning nondisclosure or perceived exposure. This is a dangerous simplification that equates a manageable chronic health condition with “criminal” intent to harm, ignoring the realities of living with HIV in the U.S. and the advances in medical treatment that reduce the risk of transmission to zero. These stigmatizing attitudes are reflected in state criminal laws that do not necessarily protect survivors of actual sexual violence effectively but are quick to criminalize individuals living with HIV under the guise of sexual offense.
Furthermore, in some jurisdictions, laws regarding sexual assault may not adequately protect survivors, focusing instead on punitive measures rather than restorative or protective ones. Conversely, HIV criminalization laws are often strictly enforced, leading to a situation where the law itself can perpetuate injustice―such as placing people on sex-offense registries when no harm has been caused except to the person who has been prosecuted. These discrepancies in legal approaches highlight the need for a more informed and balanced legal system that considers scientific evidence and the nuances of each case.
Collaboration Between Advocates
Altogether, activists and organizations dedicated to sexual assault prevention and HIV advocacy often find common ground in their work, striving to address these interconnected issues. By promoting comprehensive sexual health education, advocating for survivors’ rights, and challenging societal norms that contribute to both sexual violence and HIV stigma, these groups aim to foster a more just and informed society.
Similarly, the #MeToo movement against sexual assault and the HIV decriminalization movement share many challenges, including overcoming deep-seated stigmas and navigating a flawed U.S. legal system. As we observe Sexual Assault Awareness and Prevention Month, it’s crucial to recognize that people living with HIV facing prosecution and survivors of sexual assault are allies in the struggle for justice and dignity. By understanding the intersections and commonalities between these issues, advocates can work together more effectively to promote change, protect rights, and eliminate stigma, ensuring a fairer future for all.
Robert Suttle is a New York City-based advocacy consultant and movement leader in the global HIV community with expertise in decriminalization, human rights, and the intersection between equity and social justice.